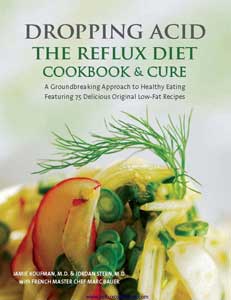
 About a year ago, I attended a cooking demonstration for a book called Dropping Acid: The Reflux Cookbook & Cure. A colleague invited me to the event after learning that I avoided coffee because it gives me heartburn.
About a year ago, I attended a cooking demonstration for a book called Dropping Acid: The Reflux Cookbook & Cure. A colleague invited me to the event after learning that I avoided coffee because it gives me heartburn.
I hoped the demonstration would give me some new ideas about what I could eat that wouldn’t give me heartburn. I had first been diagnosed with heartburn during college, after experiencing chest pain so severe it woke me up in the middle of the night. I vaguely knew that I shouldn’t eat citrus, drink excessively or eat spicy foods, but typically found it easier to pop a few Tums rather than think too much about my diet.
As Master Chef Marc Bauer demonstrated his recipes, Dr. Jamie Koufman, the principal author of Dropping Acid, also described the prevalence of acid reflux and some of its accompanying symptoms. As she spoke, I realized that I suffered from a number of other symptoms related to acid reflux in addition to heartburn: chronic hoarseness and coughing, the feeling of something stuck in my throat, and a voice that was easily fatigued. After the presentation, I was eager to speak with Dr. Koufman more, and requested an interview. After hearing about my symptoms and the sound of my raspy voice, she suggested I come to her office for treatment so that I could write my story from a patient’s perspective. I was so happy about the project that I nearly burst into tears while telling my mother about it on the phone later that night.
Dr. Koufman diagnosed me not only with Gastroesophageal reflux disease (GERD), but also with Laryngopharyngeal reflux (LPR). In other words, stomach acid was not only coming back into my esophagus, but was also reaching my voice box and throat. This not only causes the discomfort of heartburn, but also puts patients at risk for conditions like Barrett’s disease and possibly even throat cancer.
Many of the patients Dr. Koufman sees in her New York City office suffer from LPR but not the classic reflux symptom of heartburn. This condition, for which she coined the term “Silent Reflux,” is often misdiagnosed as allergies or asthma. “The first red flag is that patients come with symptoms that aren’t getting addressed by their doctors,” says Dr. Koufman. “The lung doctors really don’t recognize that reflux is in the throat all the time, and if it’s getting in the throat it’s getting in the lungs.”
She explained to me that diet alone could treat about 30 percent of her patients, but that my condition was serious enough to warrant medication as well. Dr. Koufman explained that the tissues in the throat are much more sensitive than those in the esophagus below, which means that Silent Reflux needs more aggressive treatment. “Normally diet plays a bigger role,” she says, in addition to giving me a combination of two medications to prevent reflux. “We need closer to 24-hour suppression. For that reason, we use twice daily proton pump inhibitors, before breakfast and before the evening meal, and an H2 antagonist at night.”
For the first two weeks of treatment, I followed an extremely restricted diet that was low in both acid and fat. This was easily the most challenging part of the treatment. I have always liked healthy foods, but having been always very active I’ve never really had to worry too much about what I ate. During these first weeks, patients can eat breads and starches, most vegetables, lean protein, herbs, bananas and milk. I mostly ate a lot of bananas, cereal, graham crackers and carrots. I spent a lot of time feeling pretty hungry and sorry for myself. However, my cough went away, along with the feeling of having something caught in my throat. As time went on, my hoarse voice also disappeared.
 After the first two weeks, I was allowed to start adding foods back into my diet, but continued to avoid high-acid foods like citrus and soda. I also needed to avoid eating three hours before bed, and work at eating smaller meals and snacks throughout the day. Simply eating too much at one sitting can also cause reflux. I was a little nervous about expanding my diet, adding only eggs and cheese at first. I learned that tomatoes and onions are trigger foods for me, in addition to coffee and oranges. My heartburn lessened more and more as time went on. I found the recipes in Dropping Acid to be very useful, and often used them as models to create new recipes.
After the first two weeks, I was allowed to start adding foods back into my diet, but continued to avoid high-acid foods like citrus and soda. I also needed to avoid eating three hours before bed, and work at eating smaller meals and snacks throughout the day. Simply eating too much at one sitting can also cause reflux. I was a little nervous about expanding my diet, adding only eggs and cheese at first. I learned that tomatoes and onions are trigger foods for me, in addition to coffee and oranges. My heartburn lessened more and more as time went on. I found the recipes in Dropping Acid to be very useful, and often used them as models to create new recipes.
I checked in with Dr. Koufman regularly to evaluate the progress of my condition. She uses a small flexible endoscope to evaluate the throat and voice box, a procedure that can be done without intravenous anesthesia. Thus, she was able to see the progress of my healing throat, which progressively got less swollen and inflamed.
My progress wasn’t always smooth. At one point we also made an adjustment to my medications when it appeared that I was still refluxing at night. After I got comfortable with my diet, I found it difficult to avoid eating late at night, particularly when out with friends but learned how to plan my evenings better. Now, a year after I began treatment, Dr. Koufman says I’ll soon be able to taper off the medications, and that my throat appears close to normal. Although it took quite a while to adjust to a new diet, it feels great to not suffer from heartburn or other reflux symptoms.
Over the course of the year, I spoke with many people who also suffer from reflux. What surprised me the most was how many people are given prescriptions without any mention of making changes to their diet. Of course, my story represents anecdotal evidence, but Dr. Koufman’s research shows that nearly 40 percent of Americans suffer from reflux, all of whom could benefit from lowering the amount of acid in their diets.
Also Read:
Common Myths About Acid Reflux

Hello! I just found your article – it’s incredibly informative and helpful. I have recently purchased Dr. Koufman’s books and intend to follow through with anything necessary to correct this issue (I had no idea the acid issue was THE issue, I thought my asthma was central to my problems). May I ask what change she made to the OTC meds when you realized you were still refluxing at night? I am slim & already eat a pretty healthy plant based diet – but I have made multiple errors over the years from an acid perspective (eating before bed, bending over a lot after eating, too much sugar, etc.). I will be scheduling to see an ENT here (I’m in PA). I was also wondering how your reflux is now? Thank you for the article, and any further information. Take care!
Thank You for an informative article!
I am a new owner of both of the Dr’s books.
I am surprised that she put you on PPIs for over one year! I did not expect that!
How are you now?
May we have an update please!?
Thank You!